TOP 100 SECRETS about Cardiology
1. Coronary flow reserve (the increase in coronary blood flow in response to agents that lead to
microvascular dilation) begins to decrease when a coronary artery stenosis is 50% or more luminal
diameter. However, basal coronary flow does not begin to decrease until the lesion is 80% to 90%
luminal diameter.
2. The most commonly used criteria to diagnose left ventricular hypertrophy (LVH) are R wave in V5 or
V6 + S wave in V1 or V2 > 35 mm, or R wave in lead I plus S wave in lead III > 25 mm.
3. Causes of ST segment elevation include acute myocardial infarction (MI) as a result of thrombotic
occlusion of a coronary artery, Prinzmetal angina, cocaine-induced MI, pericarditis, left ventricular (LV)
aneurysm, left bundle branch block (LBBB), LVH with repolarization abnormalities, J point elevation,
and severe hyperkalemia.
4. The initial electrocardiogram (ECG) manifestation of hyperkalemia is peaked T waves. As the hyperkalemia
becomes more profound, there may be loss of visible P waves, QRS widening, and ST segment
elevation. The preterminal finding is a sinusoidal pattern on the ECG.
5. The classic carotid arterial pulse in a patient with aortic stenosis is reduced (parvus) and delayed
(tardus).
6. The most common ECG finding in pulmonary embolus is sinus tachycardia. Other ECG findings that
can occur include right atrial (RA) enlargement (P pulmonale), right axis deviation, T-wave inversions
in leads V1 to V2, incomplete right bundle branch block (IRBBB), and a S1Q3T3 pattern (an S wave in
lead I, a Q wave in lead III, and an inverted T wave in lead III).
7. The major risk factors for coronary artery disease (CAD) are family history of premature CAD (father,
mother, brother, or sister who first developed clinical CAD at age younger than 45 to 55 for males and
at age younger than 55 to 60 for females), hypercholesterolemia, hypertension, cigarette smoking,
and diabetes mellitus.
8. Important causes of chest pain not related to atherosclerotic CAD include aortic dissection, pneumothorax,
pulmonary embolism (PE), pneumonia, hypertensive crisis, Prinzmetal angina, cardiac
syndrome X, anomalous origin of the coronary artery, pericarditis, esophageal spasm or esophageal
rupture (Boerhaave syndrome), and shingles.
9. The Kussmaul sign is the paradoxical increase in jugular venous pressure (JVP) that occurs during
inspiration. JVP normally decreases during inspiration because the inspiratory fall in intrathoracic
pressure creates a sucking effect on venous return. Kussmaul sign is observed when the right side of
the heart is unable to accommodate an increased venous return, such as can occur with constrictive
pericarditis, severe heart failure, cor pulmonale, restrictive cardiomyopathy, tricuspid stenosis, and
right ventricular (RV) infarction.
TOP 100 SECRETS
2 TOP 100 SECRETS
10. Other causes of elevated cardiac troponin, besides acute coronary syndrome and myocardial infarction,
that should be considered in patients with chest pains include PE, aortic dissection, myopericarditis,
severe aortic stenosis, and severe chronic kidney disease.
11. Prinzmetal angina, also called variant angina, is an unusual angina caused by coronary vasospasm.
Patients with Prinzmetal angina are typically younger and often female. Treatment is based primarily
on the use of calcium channel blockers and nitrates.
12. Cardiac syndrome X is an entity in which patients describe typical exertional anginal symptoms,
yet are found on cardiac catheterization to have nondiseased, normal coronary arteries.
Although there are likely multiple causes and explanations for cardiac syndrome X, it does
appear that, at least in some patients, microvascular coronary artery constriction or dysfunction
plays a role.
13. The three primary antianginal medications used for the treatment of chronic stable angina are
β-blockers, nitrates, and calcium channel blockers. Ranolazine, a newer antianginal agent, is
generally
used only as a third-line agent in patients with continued significant angina despite
traditional
antianginal therapy who have CAD not amenable to revascularization.
14. Findings that suggest a heart murmur is pathologic and requires further evaluation include the
presence of symptoms, extra heart sounds, thrills, abnormal ECG or chest radiography, diminished
or absent S2, holosystolic (or late systolic) murmur, any diastolic murmur, and all continuous
murmurs.
15. The major categories of ischemic stroke are large vessel atherosclerosis (including embolization from
carotid to cerebral arteries), small vessel vasculopathy or lacunar type, and cardioembolic.
16. Hemorrhagic strokes are classified by their location: subcortical (associated with uncontrolled
hypertension in 60% of cases) versus cortical (more concerning for underlying mass, arteriovenous
malformation, or amyloidosis).
17. Common radiographic signs of congestive heart failure include enlarged cardiac silhouette, left atrial
(LA) enlargement, hilar fullness, vascular redistribution, linear interstitial opacities (Kerley lines),
bilateral alveolar infiltrates, and pleural effusions (right greater than left).
18. Classic ECG criteria for the diagnosis of ST elevation myocardial infarction (STEMI), warranting thrombolytic
therapy, are ST segment elevation greater than 0.1 mV in at least two contiguous leads (e.g.,
leads III and aVF or leads V2 and V3) or new or presumably new LBBB.
19. Primary percutaneous coronary intervention (PCI) refers to the strategy of taking a patient who presents
with STEMI directly to the cardiac catheterization laboratory to undergo mechanical revascularization
using balloon angioplasty, coronary stents, and other measures.
20. The triad of findings suggestive of RV infarction are hypotension, distended neck veins, and clear
lungs.
21. Cessation of cerebral blood flow for as short a period as 6 to 8 seconds can precipitate syncope.
22. The most common causes of syncope in pediatric and young patients are neurocardiogenic syncope
(vasovagal syncope, vasodepressor syncope), conversion reactions (psychiatric causes), and primary
arrhythmic causes (e.g., long QT syndrome, Wolff-Parkinson-White syndrome). In contrast, elderly
patients have a higher frequency of syncope caused by obstructions to cardiac output (e.g., aortic
stenosis, PE) and by arrhythmias resulting from underlying heart disease.
TOP 100 SECRETS 3
23. Preexisting renal disease and diabetes are the two major risk factors for the development of contrast
nephropathy. Preprocedure and postprocedure hydration is the most established method of reducing
the risk of contrast nephropathy.
24. During coronary angiography, flow down the coronary artery is graded using the TIMI flow grade (flow
grades based on results of the Thrombolysis in Myocardial Infarction trial), in which TIMI grade 3 flow
is normal and TIMI grade 0 flow means there is no blood flow down the artery.
25. The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) recommends
that all adults age 20 years or older should undergo the fasting lipoprotein profile every 5 years. Testing
should include total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein
(HDL) cholesterol, and triglycerides.
26. Important secondary causes of hyperlipidemia include diabetes, hypothyroidism, obstructive liver
disease, chronic renal failure or nephrotic syndrome, and certain drugs (progestins, anabolic steroids,
corticosteroids).
27. The minimum LDL goal for secondary prevention in patients with established CAD, peripheral vascular
disease, or diabetes is an LDL less than 100 mg/dL. A goal of LDL less than 70 mg/dL should be
considered in patients with CAD at very high risk, including those with multiple major coronary risk
factors (especially diabetes), severe and poorly controlled risk factors (especially continued cigarette
smoking), and multiple risk factors of the metabolic syndrome and those with acute coronary
syndrome.
28. Factors that make up metabolic syndrome include abdominal obesity (waist circumference in men
larger than 40 inches/102 cm or in women larger than 35 inches/88 cm); triglycerides 150 mg/dL
or higher; low HDL cholesterol (less than 40 mg/dL in men or less than 50 mg/dL in women); blood
pressure 135/85 mm Hg or higher; and fasting glucose 110 mg/dL or higher.
29. Although optimal blood pressure is less than 120/80 mm Hg, the goal of blood pressure treatment
is to achieve blood pressure levels less than 140/90 mm Hg in most patients with uncomplicated
hypertension.
30. Up to 5% of all hypertension cases are secondary, meaning that a specific cause can be identified.
Causes of secondary hypertension include renal artery stenosis, renal parenchymal disease, primary
hyperaldosteronism, pheochromocytoma, Cushing disease, hyperparathyroidism, aortic coarctation,
and sleep apnea.
31. Clinical syndromes associated with hypertensive emergency include hypertensive encephalopathy,
intracerebral hemorrhage, unstable angina or acute myocardial infarction, pulmonary edema, dissecting
aortic aneurysm, or eclampsia.
32. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment
of High Blood Pressure (JNC-7) recommends that hypertensive emergencies be treated in an
intensive care setting with intravenously administered agents, with an initial goal of reducing mean
arterial blood pressure by 10% to 15%, but no more than 25%, in the first hour and then, if stable, to
a goal of 160/100 to 160/110 mm Hg within the next 2 to 6 hours.
33. Common causes of depressed LV systolic dysfunction and cardiomyopathy include CAD, hypertension,
valvular heart disease, and alcohol abuse. Other causes include cocaine abuse, collagen vascular disease,
viral infection, myocarditis, peripartum cardiomyopathy, acquired immunodeficiency syndrome
(AIDS), tachycardia-induced cardiomyopathy, hypothyroidism, anthracycline toxicity, and Chagas
disease.
4 TOP 100 SECRETS
34. The classic signs and symptoms of patients with heart failure are dyspnea on exertion (DOE), orthopnea,
paroxysmal nocturnal dyspnea (PND), and lower extremity edema.
35. Heart failure symptoms are most commonly classified using the New York Heart Association (NYHA)
classification system, in which class IV denotes symptoms even at rest and class I denotes the ability
to perform ordinary physical activity without symptoms.
36. Patients with depressed ejection fractions (less than 40%) should be treated with agents that block the
rennin-angiotensin-aldosterone system, in order to improve symptoms, decrease hospitalizations, and
decrease mortality. Angiotensin-converting enzyme (ACE) inhibitors are first-line therapy; alternate or
additional agents include angiotensin II receptor blockers (ARBs) and aldosterone receptor blockers.
37. The combination of high-dose hydralazine and high-dose isosorbide dinitrate should be used in
patients who cannot be given or cannot tolerate ACE inhibitors or ARBs because of renal function
impairment or hyperkalemia.
38. High-risk features in patients hospitalized with acute decompensated heart failure (ADHF) include
low systolic blood pressure, elevated blood urea nitrogen (BUN), hyponatremia, history of prior heart
failure hospitalization, elevated brain natriuretic peptide (BNP), and elevated troponin I or T.
39. Atrioventricular (AV) node reentry tachycardia (AVNRT) accounts for 65% to 70% of paroxysmal
supraventricular tachycardias (SVTs).
40. Implantable cardioverter defibrillators (ICDs) should be considered for primary prevention of sudden
cardiac death in patients whose LV ejection fractions remains less than 30% to 35% despite optimal
medical therapy or revascularization and who have good-quality life expectancy of at least 1 year.
41. The three primary factors that promote venous thrombosis (known together as Virchow triad ) are (1)
venous blood stasis; (2) injury to the intimal layer of the venous vasculature; and (3) abnormalities in
coagulation or fibrinolysis.
42. Diastolic heart failure is a clinical syndrome characterized by the signs and symptoms of heart failure,
a preserved LV ejection fraction (greater than 45% to 50%), and evidence of diastolic dysfunction.
43. The four conditions identified as having the highest risk of adverse outcome from endocarditis, for
which prophylaxis with dental procedures is still recommended by the American Heart Association,
are prosthetic cardiac valve, previous infective endocarditis, certain cases of congenital heart disease,
and cardiac transplantation recipients who develop cardiac valvulopathy.
44. Findings that should raise the suspicion for endocarditis include bacteremia and/or sepsis of unknown
cause, fever, constitutional symptoms, hematuria and/or glomerulonephritis and/or suspected renal
infarction, embolic event of unknown origin, new heart murmurs, unexplained new AV nodal conduction
abnormality, multifocal or rapid changing pulmonic infiltrates, peripheral abscesses, certain cutaneous
lesions (Osler nodes, Janeway lesions), and specific ophthalmic manifestations (Roth spots).
45. Transthoracic echo (TTE) has a sensitivity of 60% to 75% in the detection of native valve endocarditis. In
cases where the suspicion of endocarditis is higher, a negative TTE should be followed by a transesophageal
echo (TEE), which has a sensitivity of 88% to 100% and a specificity of 91% to 100% for native valves.
46. The most common cause of culture-negative endocarditis is prior use of antibiotics. Other causes
include fastidious organisms (Haemophilus aphrophilus, Actinobacillus actinomycetemcomitans,
Cardiobacterium hominis, Eikenella corrodens, and various species of Kingella [HACEK group]; Legionella;
Chlamydia; Brucella; and certain fungal infections) and noninfectious causes.
TOP 100 SECRETS 5
47. Indications for surgery in cases of endocarditis include acute aortic insufficiency or mitral regurgitation
leading to congestive heart failure, cardiac abscess formation or perivalvular extension,
persistence of infection despite adequate antibiotic treatment, recurrent peripheral emboli, cerebral
emboli, infection caused by microorganisms with a poor response to antibiotic treatment (e.g., fungi),
prosthetic valve endocarditis (particularly if hemodynamic compromise exists), “mitral kissing infection,”
and large (greater than 10 mm) mobile vegetations.
48. The main echocardiographic criteria for severe mitral stenosis are mean transvalvular gradient
greater than 10 mm Hg, mitral valve area less than 1 cm2, and pulmonary artery (PA) systolic pressure
greater than 50 mm Hg.
49. The classic auscultatory findings in mitral valve prolapse (MVP) is a midsystolic click and late systolic
murmur, although the click may actually vary somewhat within systole, depending on changes in LV
dimension, and there may actually be multiple clicks. The clicks are believed to result from the sudden
tensing of the mitral valve apparatus as the leaflets prolapse into the LA (LA) during systole.
50. In patients with pericardial effusions, echocardiography findings that indicate elevated intrapericardial
pressure and tamponade physiology include diastolic indentation or collapse of the RV, compression
of the RA for more than one third of the cardiac cycle, lack of inferior vena cava (IVC) collapsibility
with deep inspiration, 25% or more variation in mitral or aortic Doppler flows, and 50% or greater
variation of tricuspid or pulmonic valve flows with inspiration.
51. The causes of pulseless electrical activity (PEA) can be broken down to the H’s and T’s of PEA, which
are hypovolemia, hypoxemia, hydrogen ion (acidosis), hyperkalemia or hypokalemia, hypoglycemia,
hypothermia, toxins, tamponade (cardiac), tension pneumothorax, thrombosis (coronary and pulmonary),
and trauma.
52. Hemodynamically significant atrial septal defects (ASDs) have a shunt ratio greater than 1.5, are usually
10 mm or larger in diameter, and are usually associated with RV enlargement.
53. Findings suggestive of a hemodynamically significant coarctation include small diameter (less than
10 mm or less than 50% of reference normal descending aorta at the diaphragm), presence of collateral
blood vessels, and a gradient across the coarctation of more than 20 to 30 mm Hg.
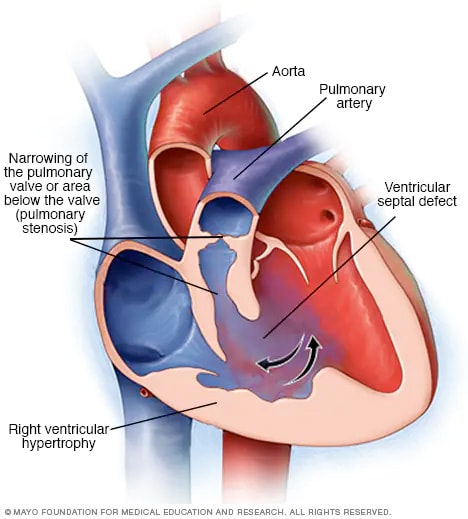
54. Tetralogy of Fallot (TOF) consists of four features: right ventricular outflow tract (RVOT) obstruction, a
large ventricular septal defect (VSD), an overriding ascending aorta, and RV hypertrophy.
55. The three Ds of the Ebstein anomaly are an apically displaced tricuspid valve that is dysplastic, with a
right ventricle that may be dysfunctional.
56. Systolic wall stress is described by the law of Laplace, which states that systolic wall stress is equal to:
(arterial pressure (p) × radius (r))/2 × thickness (h) , or σ = (p × r)/2h
57. Echocardiographic findings suggestive of severe mitral regurgitation include enlarged LA or LV, the
color Doppler mitral regurgitation jet occupying a large proportion (more than 40%) of the LA, a
regurgitant volume 60 mL or more, a regurgitant fraction 50% or greater, a regurgitant orifice
0.40 cm2 or greater, and a Doppler vena contracta width 0.7 cm or greater.
58. The seven factors that make up the Thrombolysis in Myocardial Infarction (TIMI) Risk Score are: age
greater than 65 years; three or more cardiac risk factors; prior catheterization demonstrating CAD;
ST-segment deviation; two or more anginal events within 24 hours; aspirin use within 7 days; and
elevated cardiac markers.
6 TOP 100 SECRETS
59. The components of the Global Registry of Acute Coronary Events (GRACE) Acute Cardiac Syndrome
(ACS) Risk Model (at the time of admission) are age; heart rate; systolic blood pressure, creatinine;
congestive heart failure (CHF) Killip class, ST-segment deviation; elevated cardiac enzymes and/or
markers; and presence or absence of cardiac arrest at admission.
60. Myocarditis is most commonly caused by a viral infection. Other causes include nonviral infections
(bacterial, fungal, protozoal, parasitic), cardiac toxins, hypersensitivity reactions, and systemic disease
(usually autoimmune). Giant cell myocarditis is an uncommon but often fulminant form of myocarditis
characterized by multinucleated giant cells and myocyte destruction.
61. Initial therapy for patients with non–ST segment elevation acute coronary syndrome (NSTEACS)
should include antiplatelet therapy with aspirin and with either clopidogrel, ticagrelor, or a
glycoprotein
IIb/IIIa inhibitor, and antithrombin therapy with either unfractionated heparin, enoxaparin,
fondaparinux, or bivalirudin (depending on the clinical scenario).
62. Important complications in heart transplant recipients include infection, rejection, vasculopathy (diffuse
coronary artery narrowing), arrhythmias, hypertension, renal impairment, malignancy (especially
skin cancer and lymphoproliferative disorders), and osteoporosis (caused by steroid use).
63. The classic symptoms of aortic stenosis are angina, syncope, and those of heart failure (dyspnea,
orthopnea, paroxysmal nocturnal dyspnea, edema, etc.). Once any of these symptoms occur, the
average survival without surgical intervention is 5, 3, or 2 years, respectively.
64. Class I indications for aortic valve replacement (AVR) include (1) development of symptoms in patients
with severe aortic stenosis; (2) an LV ejection fraction of less than 50% in the setting of severe aortic
stenosis; and (3) the presence of severe aortic stenosis in patients undergoing coronary artery bypass
grafting, other heart valve surgery, or thoracic aortic surgery.
65. The major risk factors for venous thromboembolism (VTE) include previous thromboembolism, immobility,
cancer and other causes of hypercoagulable state (protein C or S deficiency, factor V Leiden,
antithrombin deficiency), advanced age, major surgery, trauma, and acute medical illness.
66. The Wells Score in cases of suspected pulmonary embolism (PE) includes deep vein
thrombosis
(DVT) symptoms and signs (3 points); PE as likely as or more likely than alternative
diagnosis (3 points); heart rate greater 100 beats/min (1.5 points); immobilization or surgery in
previous 4 weeks (1.5 points); previous DVT or PE (1.5 points); hemoptysis (1.0 point); and cancer
(1 point).
67. The main symptoms of aortic regurgitation (AR) are dyspnea and fatigue. Occasionally patients
experience angina because reduced diastolic aortic pressure reduces coronary perfusion pressure,
impairing coronary blood flow. Reduced diastolic systemic pressure may also cause syncope or
presyncope.
68. The physical findings of AR include widened pulse pressure, a palpable dynamic LV apical beat that
is displaced downward and to the left, a diastolic blowing murmur heard best along the left sternal
border with the patient sitting upright and leaning forward, and a low-pitched diastolic rumble heard
to the LV apex (Austin Flint murmur).
69. Class I indications for aortic valve replacement in patients with AR include (1) the presence of symptoms
in patients with severe AR, irrespective of LV systolic function; (2) chronic severe AR with LV
systolic dysfunction (ejection fraction 50% or less), even if asymptomatic; and (3) chronic, severe AR
in patients undergoing coronary artery bypass grafting (CABG), other heart valve surgery, or thoracic
aortic surgery.
TOP 100 SECRETS 7
70. Cardiogenic shock is a state of end-organ hypoperfusion caused by cardiac failure characterized by
persistent hypotension with severe reduction in cardiac index (less than 1.8 L/min/m2) in the presence
of adequate or elevated filling pressure (LV end-diastolic pressure 18 mm Hg or higher or RV
end-diastolic pressure 10 to 15 mm Hg or higher).
71. The rate of ischemic stroke in patients with nonvalvular atrial fibrillation (AF) is about two to seven
times that of persons without AF, and the risk increases dramatically as patients age. Both paroxysmal
and chronic AF carry the same risk of thromboembolism.
72. In nuclear cardiology stress testing, a perfusion defect is an area of reduced radiotracer uptake in the
myocardium. If the perfusion defect occurs during stress and improves or normalizes during rest, it is
termed reversible and usually suggests the presence of inducible ischemia, whereas if the perfusion
defect occurs during both stress and rest, it is termed fixed and usually suggests the presence of scar
(infarct).
73. The main organ systems that need to be monitored with long-term amiodarone therapy are the lungs,
the liver, and the thyroid gland. A chest radiograph should be obtained every 6 to 12 months, and
liver function tests (LFTs) and thyroid function tests (thyroid-stimulating hormone [TSH] and free T4)
should be checked every 6 months.
74. The target international normalized ratio (INR) for warfarin therapy in most cases of cardiovascular
disease is 2.5, with a range of 2.0 to 3.0. In certain patients with mechanical heart valves (e.g., older
valves, mitral position), the target is 3.0 with a range of 2.5 to 3.5.
75. Lidocaine may cause a variety of central nervous system symptoms including seizures, visual disturbances,
tremors, coma, and confusion. Such symptoms are often referred to as lidocaine toxicity.
The risks of lidocaine toxicity are increased in elderly patients, those with depressed LV function, and
those with liver disease.
76. The most important side effect of the antiarrhythmic drug sotalol is QT-segment prolongation leading
to torsades de pointes.
77. The major complications of percutaneous coronary intervention (PCI) include periprocedural MI,
acute stent thrombosis, coronary artery perforation, contrast nephropathy, access site complications
(e.g., retroperitoneal bleed, pseudoaneurysm, arteriovenous fistula), stroke, and a very rare need for
emergency CABG.
78. The widely accepted hemodynamic definition of pulmonary arterial hypertension (PAH) is a mean
pulmonary arterial pressure of more than 25 mm Hg at rest or more than 30 mm Hg during exercise,
with a pulmonary capillary or LA pressure of less than 15 mm Hg.
79. Acute pericarditis is a syndrome of pericardial inflammation characterized by typical chest pain, a
pathognomonic pericardial friction rub, and specific electrocardiographic changes (PR depression,
diffuse ST-segment elevation).
80. Conditions associated with the highest cardiac risk in noncardiac surgery are unstable coronary
syndromes (unstable or severe angina), decompensated heart failure, severe valvular disease (particularly
severe aortic stenosis), and severe arrhythmias.
81. General criteria for surgical intervention in cases of thoracic aortic aneurysm are, for the ascending
thoracic aorta, aneurysmal diameter of 5.5 cm (5.0 cm in patients with Marfan syndrome), and
for the descending thoracic aorta, aneurismal diameter of 6.5 cm (6 cm in patients with Marfan
syndrome).
8 TOP 100 SECRETS
82. Cardiac complications of advanced AIDS in untreated patients include myocarditis and/or cardiomyopathy
(systolic and diastolic dysfunction), pericardial effusion/tamponade, marantic (thrombotic)
or infectious endocarditis, cardiac tumors (Kaposi sarcoma, lymphoma), and RV dysfunction from
pulmonary hypertension or opportunistic infections. Complications with modern antiretroviral therapy
(ART) include dyslipidemias, insulin resistance, lipodystrophy, atherosclerosis, and arrhythmias.
83. The radiation dose of a standard cardiac computed tomography (CT) angiography depends on a
multitude of factors and can range from 1 mSv to as high as 30 mSv. This compares to an average
radiation dose from a nuclear perfusion stress test of 6 to 25 mSv (or as high as more than 40 mSv
in thallium stress/rest tests) and an average dose from a simple diagnostic coronary angiogram of
approximately 5 mSv.
84. The ankle-brachial index (ABI) is the ankle systolic pressure (as determined by Doppler examination)
divided by the brachial systolic pressure. An abnormal index is less than 0.90. The sensitivity
is approximately 90% for diagnosis of peripheral arterial disease (PAD). An ABI of 0.41 to 0.90 is
interpreted as mild to moderate peripheral arterial disease; an ABI of 0.00 to 0.40 is interpreted as
severe PAD.
85. Approximately 90% of cases of renal artery stenosis are due to atherosclerosis. Fibromuscular
dysplasia (FMD) is the next most common cause.
86. In very general terms, in cases of carotid artery stenosis, indications for carotid endarterectomy
(CEA) are: (1) symptomatic stenosis 50% to 99% diameter if the risk of perioperative stroke or death
is less than 6%; and (2) asymptomatic stenosis greater than 60% to 80% diameter if the expected
perioperative stroke rate is less than 3%.
87. The most common cardiac complications of systemic lupus erythematosus (SLE) are pericarditis,
myocarditis, premature atherosclerosis, and Libman-Sacks endocarditis.
88. Cardiac magnetic resonance imaging (MRI) can be performed in most patients with implanted cardiovascular
devices, including most coronary and peripheral stents, prosthetic heart valves, embolization
coils, intravenous vena caval filters, cardiac closure devices, and aortic stent grafts. Pacemakers and
implantable cardioverter defibrillators are strong relative contraindications to MRI scanning, and scanning
of such patients should be done under specific delineated conditions, only at centers with expertise
in MRI safety and electrophysiology, and only when MRI imaging in particular is clearly indicated.
89. The clinical manifestations of symptomatic bradycardia include fatigue, lightheadedness, dizziness,
presyncope, syncope, manifestations of cerebral ischemia, dyspnea on exertion, decreased exercise
tolerance, and congestive heart failure.
90. Second-degree heart block is divided into two types: Mobitz type I (Wenckebach) exhibits progressive
prolongation of the PR interval before an atrial impulse (P wave) is not conducted, whereas Mobitz
type II exhibits no prolongation of the PR interval before an atrial impulse is not conducted.
91. Temporary or permanent pacing is indicated in the setting of acute MI, with or without symptoms, for
(1) complete third-degree block or advanced second-degree block that is associated with block in the
His-Purkinje system (wide complex ventricular rhythm) and (2) transient advanced (second-degree or
third-degree) AV block with a new bundle branch block.
92. Cardiac resynchronization therapy (CRT) refers to simultaneous pacing of both ventricles (biventricular,
or Bi-V, pacing). CRT is indicated in patients with advanced heart failure (usually NYHA class III
or IV), severe systolic dysfunction (LV ejection fraction 35% or less), and intraventricular conduction
delay (QRS less than 120 ms) who are in sinus rhythm and have been on optimal medical therapy.
TOP 100 SECRETS 9
93. Whereas the left internal mammary artery (LIMA), when anastomosed to the left anterior descending
artery (LAD), has a 90% patency at 10 years, for saphenous vein grafts (SVGs), early graft stenosis or
occlusion of up to 15% can occur by 1 year, with 10-year patency traditionally cited at only 50% to
60%.
94. Myocardial contusion is a common, reversible injury that is the consequence of a nonpenetrating
trauma to the myocardium. It is detected by elevations of specific cardiac enzymes with no evidence
of coronary occlusion and by reversible wall motion abnormalities detected by echocardiography.
95. Causes of restrictive cardiomyopathy include infiltrative diseases (amyloidosis, sarcoidosis, Gaucher
disease, Hurler disease), storage diseases (hemochromatosis, glycogen storage disease, Fabry
disease), and endomyocardial involvement from endomyocardial fibrosis, radiation, or anthracycline
treatment.
96. Classical signs for cardiac tamponade include the Beck triad of (1) hypotension caused by decreased
stroke volume, (2) jugulovenous distension caused by impaired venous return to the heart, and
(3) muffled heart sounds caused by fluid inside the pericardial sac, as well as pulsus paradoxus and
general signs of shock, such as tachycardia, tachypnea, and decreasing level of consciousness.
97. The most common tumors that spread to the heart are lung (bronchogenic) cancer, breast cancer,
melanoma, thyroid cancer, esophageal cancer, lymphoma, and leukemia.
98. Primary cardiac tumors are extremely rare, occurring in one autopsy series in less than 0.1% of
subjects. Benign primary tumors are more common than malignant primary tumors, occurring
approximately three times as often as malignant tumors.
99. The Westermark sign is the finding in pulmonary embolism of oligemia of the lung beyond the
occluded vessel. If pulmonary infarction results, a wedge-shaped infiltrate (Hampton’s hump) may be
visible.
100. Patients with cocaine-induced chest pain should be treated with intravenous benzodiazepines,
which can have beneficial hemodynamic effects and relieve chest pain, and aspirin therapy, as well
as nitrate therapy if the patient remains hypertensive. β-blockers (including labetalol) should not be
administered in the acute setting of cocaine-induced chest pain